Abstract
STUDY QUESTION:
SUMMARY ANSWER:
WHAT IS KNOWN ALREADY:
STUDY DESIGN, SIZE, DURATION:
PARTICIPANTS/MATERIALS, SETTING, METHODS:
MAIN RESULTS AND THE ROLE OF CHANCE:
LIMITATIONS, REASONS FOR CAUTION:
WIDER IMPLICATIONS OF THE FINDINGS:
The truth is, being a parent is a life changer; it offers couples an entirely different perspective on why they wake up every day. And people who are deprived of this blessing can come to Care Womens Centre. Care Womens Centre is one of the Best fertility hospitals in Indore to get IVF treatments and fulfill their inherent desire to be a parent. Care Womens Centre is provide the world class infertility treatment, test tube baby treatment, IUI treatment and ICSI treatment in Indore. Dr Shweta Kaul Jha is Best IVF specialist at Care Womens Centre. If you are Search for the Best centre for IVF in Indore come to Care Womens Centre. Book an appointment today call now +918889016663 and visit https://www.carewomenscentre.com for more information.
STUDY QUESTION:
Does the perception of failure without a solution or way forward of infertile couples have a mediator role between the importance couples attribute to parenthood and depressive symptoms?
SUMMARY ANSWER:
The perception of failure without a solution or way forward, assessed by feelings of entrapment and defeat, mediates the effect of the importance of parenthood on depressive symptoms of infertile men and women.
WHAT IS KNOWN ALREADY:
Research has documented that the heightened importance of parenthood affects infertile couples' adjustment to infertility and medical treatments. However, it remains unclear which psychological mechanisms and perceptions may underlie the association between having parenthood as a nuclear aspect of life and presenting depressive symptoms related to difficulties in accomplishing that important life goal. Although these links have been scantly addressed in infertility, previous studies have pointed to the role that perceptions of defeat and entrapment have in several psychopathological conditions.
STUDY DESIGN, SIZE, DURATION:
The study was cross-sectional. Couples pursuing medical treatment for their fertility problems were invited to participate by their doctors in several public and private clinics. Data collection took place between July 2009 and 2011.
PARTICIPANTS/MATERIALS, SETTING, METHODS:
One hundred forty-seven infertile couples consented to participate in the study. Both couple members (147 women and 147 men) completed a set of self-report instruments for the assessment of depressive symptoms, perceptions of defeat and entrapment, importance of parenthood and rejection of a childfree lifestyle. Analyses were conducted through Structural Equation Modeling and followed a dyadic analysis strategy, allowing for controlling the interdependence of the data.
MAIN RESULTS AND THE ROLE OF CHANCE:
The hypothesized tested model showed a very good fit to the data [(χ(2) = 68.45, P = 0.014, comparative fit index = 0.98, standardized root-mean-square residual = 0.06 and root mean square error of approximation = 0.06] and explained 67 and 58% of the variability in depressive symptoms in women and men, respectively. Results revealed that the importance of parenthood does not have a direct effect on depressive symptoms of infertile men and women, but an indirect effect, by affecting the perception of having failed and not being able to solve it or move forward [women: estimate for indirect effect: 0.38 (bias corrected (BC) 95% confidence interval (CI) = 0.25; 0.56; P < 0.001); men: estimate for indirect effect: 0.23 (BC 95% CI = 0.06; 0.40; P = 0.013)].
LIMITATIONS, REASONS FOR CAUTION:
The study was cross-sectional, which does not allow for the establishment of causality. Another limitation is the heterogeneity of the sample, as participants were recruited at various stages of their fertility care. In addition, due to the specific nature of the variables, further studies are needed to establish exactly how the relationship between defeat and entrapment and depression operates, as the mechanism may be bidirectional.
WIDER IMPLICATIONS OF THE FINDINGS:
This study emphasizes the role of perceptions of defeat and entrapment on the psychological adjustment to infertility and assisted reproduction. These emotional processes should be taken into consideration and targeted in psychological interventions of couples undergoing medical treatments for infertility. In fact, although parenthood may be perceived as a core purpose for many couples dealing with difficulties in conceiving, it is only when these difficulties are experienced as failures without a resolution and as inescapable, that couples are prone to develop depressive symptoms.
The truth is, being a parent is a life changer; it offers couples an entirely different perspective on why they wake up every day. And people who are deprived of this blessing can come to Care Womens Centre. Care Womens Centre is one of the Best fertility hospitals in Indore to get IVF treatments and fulfill their inherent desire to be a parent. Care Womens Centre is provide the world class infertility treatment, test tube baby treatment, IUI treatment and ICSI treatment in Indore. Dr Shweta Kaul Jha is Best IVF specialist at Care Womens Centre. If you are Search for the Best centre for IVF in Indore come to Care Womens Centre. Book an appointment today call now +918889016663 and visit https://www.carewomenscentre.com for more information.
Online Book an appointment :- https://www.carewomenscentre.com/appointment/
Please go through our social media :
like our page to no more about ivf
Facebook : https://www.facebook.com/CareWomensCentre/
Please do follow on Instagram
Instagram : https://www.instagram.com/carewomenscentre/
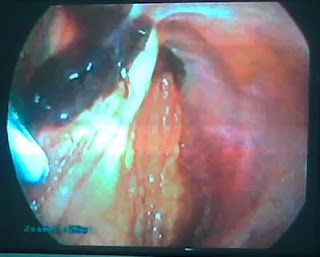
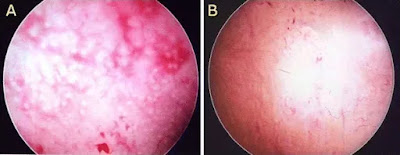
To More Post: Live twin birth after successful treatment of a ruptured heterotopic pregnancy by laparoscopy