Abstract
Transvaginal laparoscopy offers an accurate and minimally invasive method for the exploration of the female pelvis in patients with infertility. Access to the pouch of Douglas is gained through a simple needle puncture technique of the posterior fornix using a pre-warmed watery solution as the distension medium. A review of recently published papers and our own experience illustrate the safety of the technique. Transvaginal laparoscopy can be considered as one of the first and safest examples of the recent developments in natural orifice transluminal endoscopic surgery (NOTES).
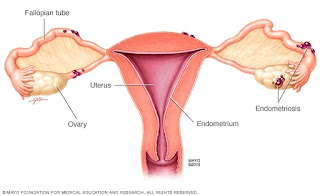
Introduction
Transvaginal laparoscopy is today accepted as a feasible technique for the investigation of female
fertility with the capacity to predict spontaneous ongoing pregnancy comparable to that of laparoscopy. The technique uses saline as the distension medium and is generally performed in an outpatient setting under intravenous sedation or local anesthesia [1, 2].
Transvaginal access has previously been used in culdoscopy, as introduced by Decker and Cherry [3] in the US and Palmer in Europe [4], but was abandoned in the 1970s, particularly when studies suggested that the transabdominal access was superior over transvaginal access for the performance of tubal sterilization [5, 6]. Recently, the Editorial Board of the American Association of Gynecologic Laparoscopists [7] expressed the fear that, after transvaginal access, 1% of
infertility patients would develop peritonitis and pelvic abscess. The fear was based on the statement that vaginal tubal sterilization carried with it a 1% abscess rate when performed in an operating room, even with the administration of prophylactic antibiotics. It is questionable on which data this statement has been based and whether it is supported by old and recent data.
Palmer [4] admitted that, after posterior colpotomy, pelvic abscesses are possible and 2% of the sterilizations fail because of fistulization of the ampulla. Whitaker [8] reviewed a series of 585 tubal ligations by colpotomy within a private-practice setting in the US. In his series, no vaginal cuff hematoma and cuff abscess requiring incision and drainage occurred. Gupta et al. [9] analyzed a series of 608 women admitted to the Department of Obstetrics and Gynecology in Chandigarth, India. No prophylactic antibiotics were given and follow-ups occurred at regular intervals up to 12 months. Two cases of serious complications, including one abscess with fistula and one pelvic peritonitis, occurred. In a review of 50,151 laparoscopies, Brosens et al. [10] reported that diagnostic laparoscopy was associated with a 0.08% risk of bowel injury. However, up to 15% of the injuries are not diagnosed during laparoscopy and one of five cases of delayed diagnosis resulted in death [11–13].
In a multinational retrospective survey in 2001, we reported on a series of 3,667 procedures of transvaginal pelvic endoscopies in infertile patients without obvious pelvic pathology [14]. Full-thickness bowel injury occurred in 24 (0.65%) procedures. After an initial experience of 50 procedures, the prevalence of bowel injury was 0.25%. However, all injuries were diagnosed during the procedure and 22 (92%) were managed conservatively without consequences. Both the type of lesion and the risk of delayed diagnosis suggest that the transvaginal access in laparoscopy is associated with a minor risk of bowel injury that, under strict conditions, is treated conservatively. The purpose of this review is to evaluate the risk of bowel injury during transvaginal laparoscopy in recent publications.
Survey design
Using the Pubmed and Scopus searches, we traced 27 original papers on diagnostic transvaginal pelvic endoscopy published between 2000 and 2007 in peer-reviewed journals. We excluded recent publications from the pioneering centers to exclude overlapping data and to include results from new centers with their initial experience. With regard to publications in languages such as Japanese and Polish, data were collected from the available English abstract.
Instrumentation
Transvaginal laparoscopy is performed using a combined system of a Veress needle and trocar with a 3.9-mm outside diameter and a semi-rigid endoscope of 2.7 or 2.9 mm, as developed by Karl Storz GmbH & Co., Tuttlingen, Germany [15–20]. Fertiloscopy is defined as the combination in one investigation of transvaginal hydropelviscopy, dye test, optional salpingoscopy, and hysteroscopy [21]. The slightly different instrumentation as developed by Soprane S.A., Lyon, France, has an outer diameter of 6 mm.
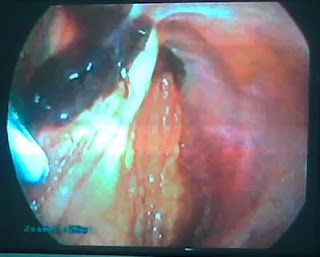
Complications
The 27 publications on transvaginal laparoscopy and fertiloscopy represented a total of 2,843 procedures (Table 1). Access was achieved according to 11 publications, each reporting on more than 50 procedures between 89% and 100%, with a mean of 94%. Access failed in 6% of the cases and the reasons included retroverted uterus, dense adhesions, adnexal mass in the cul-de-sac, nodular retrocervical endometriosis, and obesity.
No major complication, such as life-threatening hemorrhage, bowel injury requiring surgery, sepsis, or abscess formation, occurred. Minor complications occurred in 21 (0.74%) patients (Table 2). These complications included bowel injury in 10 cases (0.35%). All were treated conservatively with antibiotics. Hemorrhage requiring compression or a stitch was reported in six cases, inadvertent puncture of the posterior uterine wall in three cases, and suspected pelvic infection treated with antibiotics in two cases. No long-term or delayed complications were reported.
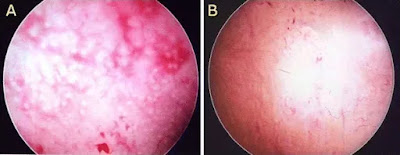
Prevention of complications
Previous research has shown that, after initial experience with 50 procedures, the risk of bowel injury decreases significantly. The findings of our previous survey [14] clearly demonstrated a decrease in incidence in bowel damage from 1.3% in the first 50 cases to 0.25% once more experience had been gained. Also, in their series, Verhoeven et al. [48] reported a reduced incidence of 0.1% once more than 50 procedures have been performed. However, even in experienced hands, injury during blind access cannot be fully avoided. Sobek et al. [23] recommended ultrasonographically guided transvaginal hydrolaparoscopy to increase the safety of the procedure and decrease the difficulty of access. With this method, no bowel injury occurred in a consecutive series of 460 patients. Mgaloblishvili et al. [22] proposed to proceed first with hysteroscopy using saline for partial filling of the pouch of Douglas, followed by sonohysterosalpingography to clearly visualize and assess the fornix and the pouch of Douglas. Cancellation for transvaginal pelvic endoscopy included:
- Complete obliteration of the pouch of Douglas
- Thickening of the posterior fornix by dilated vessels, retro-cervical endometriosis, or adipose tissue
- Dense adhesions in the pouch of Douglas
- Presence of organs such as one or both ovaries, fallopian tubes, intestinal loops, myomatous nodule, or retroverted uterus
In a series of 827 women, cancellation was indicated in six cases after hysteroscopy and in 135 cases after sonohysterosalpingography. No complications occurred in the remaining 702 patients.
Comments
The current findings support the conclusion of the previous report by Gordts et al. [14] that transvaginal access using a small-diameter endoscope for the exploration of the pelvis in infertility is a safe procedure. In contrast with transabdominal access in standard laparoscopy, delayed diagnosis of bowel injury resulting in sepsis or death has not been described. Moreover, bowel injury caused by the small-diameter instrument used in transvaginal pelvic endoscopy can be treated expectantly, although antibiotics are administered in most cases. This, however, will not exclude that inadvertent manipulation may cause a large lesion that requires surgical repair. In the absence of leakage, expectant management with the prophylactic use of antibiotics is apparently justified.

It is unclear as to which literature the statement by Hunt et al. [7] that culdoscopic access is associated with a 1% risk of sepsis has been based. Review of the early literature learns that the current findings on the risks of transvaginal access in women with infertility are in full agreement with the older literature on the risks of diagnostic culdoscopy. Riva et al. [49] published a consecutive series of 2,850 cases with 3.7% failure of access and a complication rate of 1.4%. Eleven recto-sigmoid perforations occurred (Table 3). The lesions were extra-peritoneal and were closed immediately through the colpotomy site, and the culdoscopy procedure was discontinued. Follow-up examination revealed no complications referable to these recto-sigmoid injuries. Diamond [50] used improved instrumentation and brighter illumination with fiber optics and published in 1978 a continuous series of 4,000 outpatient procedures of diagnostic culdoscopy in infertility. In his consecutive series of 4,000 culdoscopies performed between 1968 and 1978, no death occurred. Bleeding was prolonged and required suturing in six patients. Pelvic infection occurred in three cases, despite the routine use of antibiotics, and one patient developed a pelvic abscess. Inadvertent punctures were made into the rectum in five cases, all of them occurring in the first five years of the series and none later. None of the patients required hospitalization or laparotomy; all were treated with antibiotics and conservative therapy. No inadvertent puncture of other viscera occurred. In four patients, the puncture of ovarian cysts that had prolapsed into the cul-de-sac occurred. Diamond [50] concluded that, with proper preparation and organization, diagnostic culdoscopy could be carried out as a routine procedure in any adequately equipped outpatient facility in or outside the hospital. It is safe, effective, and rapid, taking an experienced physician and team no more than 10 or 15 min to perform. He proposed that outpatient culdoscopy should be returned to gynecologic training programs. With regard to the available data in the literature, the statement of the Editorial Board of the American Association of Gynecologic Laparoscopists is, therefore, astonishing. We would agree with Hunt et al. [7] that a thousand, or even several thousand, cases are required to make a statement on the safety of a new technique. The world literature during the last 40 years includes many thousands of procedures and has consistently endorsed the safety of transvaginal access in diagnostic pelvic endoscopy in women with infertility.

In infertility exploration, transvaginal laparoscopy is one of the first applications of the recent developments in natural orifice transluminal endoscopic surgery (NOTES) [51]. Considering the previously discussed results, the technique should deserve a more widespread use as an ambulatory diagnostic tool in the exploration of the infertile patient.
Please go through our social media :
like our page to no more about ivf
Please do follow on Instagram